Message from the Chief Nursing Officer
Dear Colleagues,
As our Stanford network of care expands, we continue to lead at the national and global forefront of this new era in healthcare, developing transformational professional opportunities for nurses. Whether in the inpatient or ambulatory setting, our innovative nurses are driving excellent patient care outcomes and are positively impacting the lives of our patients and our community. There is no better place to serve than as a nurse at SHC, an environment where compassion embraces science to heal humanity, one patient at a time.
Warm Regards,
Dale Beatty, DNP, RN, NEA-BC
What's New at Stanford Nursing
New Fellows of the American Academy of Nursing (FAAN)
Congratulations to Dr. Dale E. Beatty, DNP, RN, NEA-BC, WCS Caritas Coach®, DR. Michelle Y. Williams, PhD, RN, and DR. Cassendra A Munro, PhD, RN, CNOR of Stanford Health Care for being selected as new Fellows of the American Academy of Nursing (FAAN).
Stanford Medicine: News Center Four Stanford Medicine nursing leaders honored by American Academy of Nursing
FAAN is nursing’s highest academic and leadership honor, with approximately 3,000 Nursing Fellows in the world out of 4.2 million nurses in the USA and 27 million nurses globally.
This prestigious induction by the American Academy of Nursing recognizes the extraordinary contributions to improving health through generating, synthesizing, and disseminating nursing knowledge, representing today’s thought leaders and the diversity of our profession’s policy leaders, practitioners, educators, and innovators.
Beatty, DNP, is Stanford Health Care’s chief nurse executive and vice president of patient care services. He is president of the Association of California Nurse Leaders and past president of the Illinois Organization of Nurse Leaders. His professional impact is on practice-policy leadership.
Munro, PhD, is a nurse scientist who will be inducted to the academy for her lifetime research in perioperative nursing care and the development of the Munro pressure injury risk assessment scale for perioperative patients as well as the Munro scale curriculum.
Williams, PhD, is Stanford Health Care’s inaugural associate chief nursing officer of patient care services research and health equity. Williams, a clinical associate professor of medicine in primary care and population health, has been instrumental in building the Office of Research Patient Care Services.
Showcasing the latest in SHC professional excellence
Transformational
Leadership
New Knowledge
and Innovation
Exemplary Professional
Practice
Structural
Empowerment
PPM
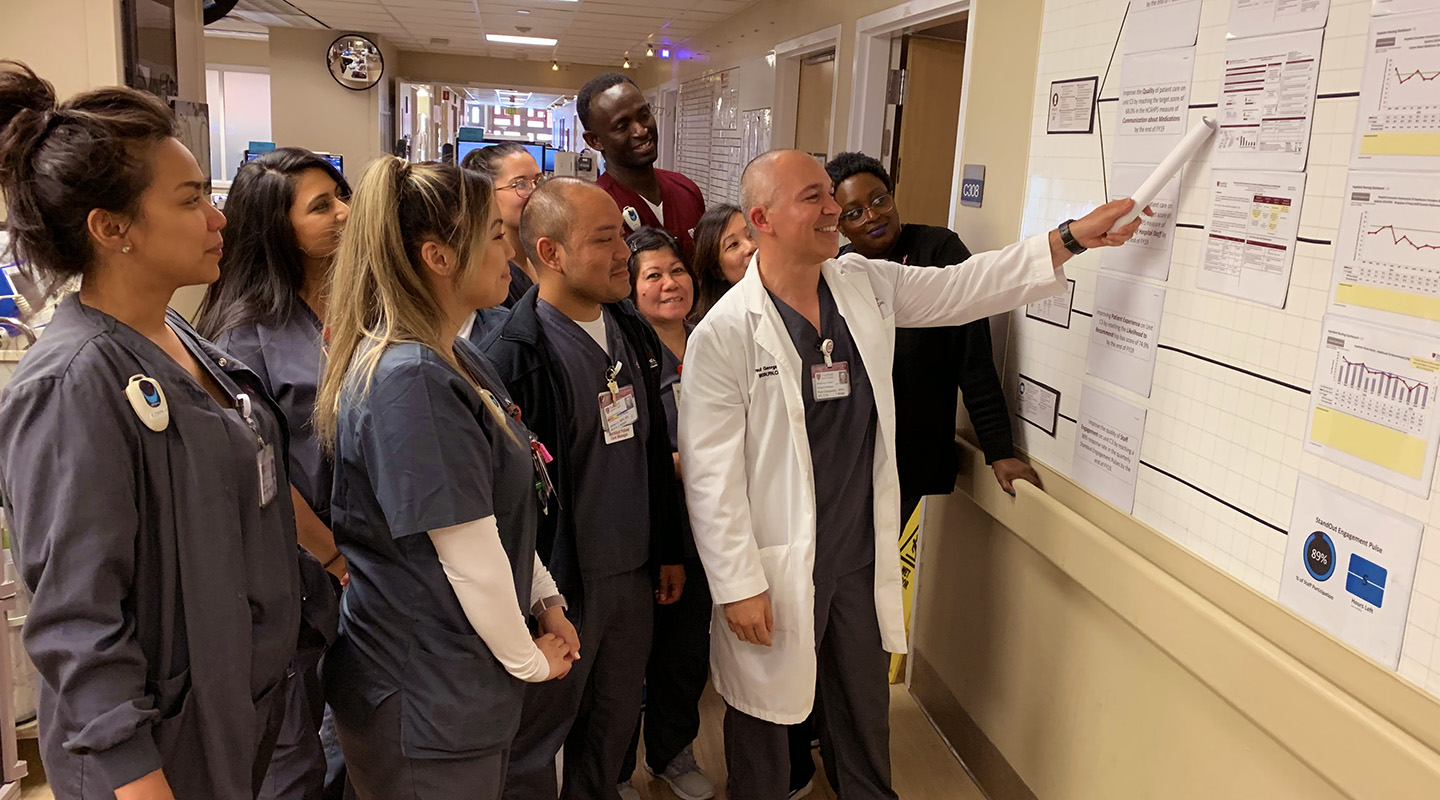
The SHC Professional Practice Model (PPM) illustrates how nurses support the organization's mission, vision, and national professional standards of nursing practice. Symbolizing our patient-centered beliefs and values, the PPM exemplifies nurse autonomy over clinical practice and the practice environment, depicting effective communication between interprofessionals to result in high-quality patient care.
Magnet
The American Nurses Credentialing Center (ANCC) Magnet Model provides a framework for clinical, operational, and leadership practice, serving as a roadmap for Stanford Nursing's ongoing pursuit toward nursing excellence.
Learn more about SHC's exciting Magnet Journey toward a 4th redesignation in 2020!
Public Notice of Scheduled Site Visit by ANCC Magnet Recognition Program Appraisers »
Watson Caring Science Institute
Beginning in 2007, SHC embraced Jean Watson's transformative Watson Caring Science Institute theory of human caring and love. This intertwining of the Watson Caring Science Institute theories with nursing practice translates into increased intentionality and a deepening of authentic presence; thereby renewing nurse relationships through universal, ethical, and person-centered care.
EMPLOYEE RESOURCES
Thanks for Joining Us! Healthcare Con 2023
Thanks for joining us at Healthcare Con 2023! Keep an eye out for the Save the Date announcemnet for the 2024 event and the Call for Abstracts coming this fall 2023. See you next time!
Healthcare Con is an interprofessional conference developed to showcase the latest in research, innovation, quality and evidence-based healthcare improvement projects. View 2023 program agenda.
Visit the Healthcare Con page for more information about the conference.
2024 Event: Coming Soon
Awards
Why Stanford Nursing?
Stanford Nurses are recognized as bold leaders, compassionate healers, educators, and mentors, providing the highest standards of excellence in care while generating long-term impressions that continue to set SHC apart as the best place to work and thrive. Stanford Nursing offers a wide array of career advancement opportunities, access to the latest technologies and health care innovations, and boasts a workplace culture that encourages personal growth and work-life balance, while honoring its commitment to delivering evidence-based and patient-centered care.
Join our team of dedicated professionals and transform your nursing practice!
Social Media
CONNECT WITH US!
Follow us on social media to see what we’re sharing with the rest of the world. #STANFORDNURSING
#SHCNURSES